My desire is to fill your heart, your home and your life with timeless memories that tells a story & reminds you of those little moments of today that become memories for tomorrow.
Welcome to my blog!
I'm Reshma
Family
Maternity
Newborn
Choose a blog
Category
make your most precious memories last
travel
stay connected with Heartfelt Updates
Join our private list
Be the first to know when we share special details, updates and musings about motherhood, life and more.
Join here

How I Discovered I Had Gestational Diabetes
When I was pregnant with my first, I felt incredibly fortunate: a textbook-smooth pregnancy, no nausea, working right up to the morning of labor (six days past my due date!), other than a lot of heartburn and him arriving late, it was a good pregnancy.
But when I was pregnant with my daughter, I knew it wouldn’t be as easy: I was a bit older, already had a toddler, and life was busier but I didn’t expect how hard it would get.
The Routine Test That Changed Everything
My first trimester sailed by smoothly. At about 26–28 weeks I took the routine glucose screening for gestational diabetes (GD). You fast, have your blood drawn, drink the sugary solution, wait an hour, get drawn again, then again after another hour. I didn’t worry – I eat well, exercise, and rarely crave sweets, blood sugar was never an issue.
But then I got that call: one of the three readings was out of range. They told me I had Gestational Diabetes.
I was in denial. How could I have it? I eat healthy. I move regularly. Yet, the diagnosis stood: I needed to enter the GD program. I figured it would be brief—“we’ll see you in a week or two, you’ll be fine” was my internal narrative.
What is Gestational Diabetes (GD)?
In the U.S., roughly 8 %–10 % of pregnancies are affected by gestational diabetes; globally the rate is closer to 14 %.
GD happens when your body has a difficult time using insulin during pregnancy. Extra sugar circulates and crosses the placenta. This triggers the baby’s pancreas to make extra insulin and results in added energy stored as fat — which can lead to risks for both mom and baby.
The Diet & Monitoring Plan
My entire meal plan and eating habits had to change. Six small meals a day. High protein, low carb with two major rules:
- A very small breakfast right after waking up.
- A high-protein bedtime snack right before bed.
Every meal had a carb-protein-fat target but the biggest thing to be aware of was the carb intake.
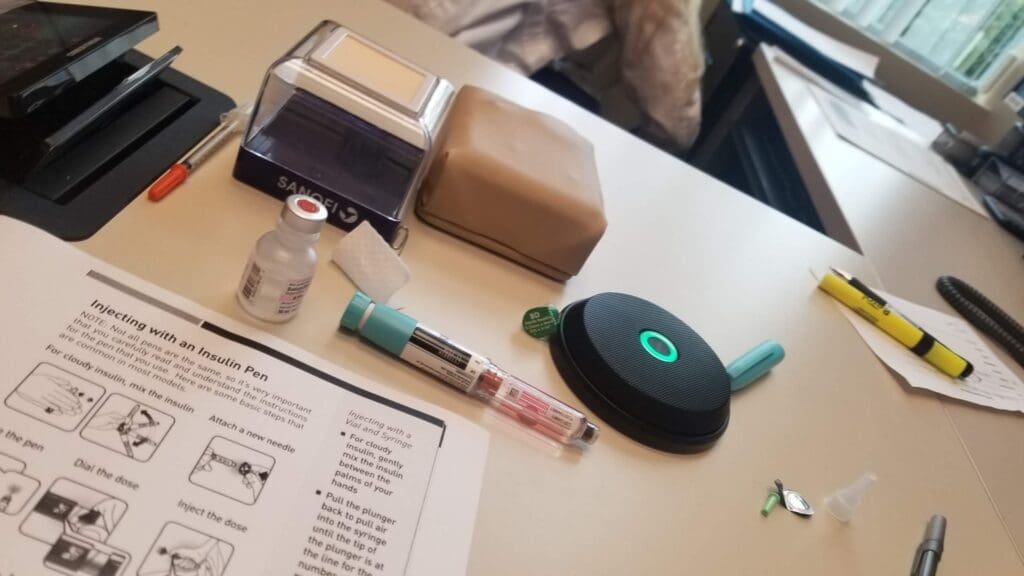
Next: blood-glucose checking 4 times a day (after each meal) with a meter. Overwhelming? Yes. Stressful? Absolutely. But necessary.
After two weeks following the diet and monitoring, they reviewed the pattern. My fasting number refused to budge. No matter how I tweaked diet or exercise, it stayed high. That meant I had progressed to what they called “type 2 gestational diabetes” — meaning I would require insulin. I felt like I failed my body—and my baby, and if you’ve been there, you know what that feels like.
Choosing Insulin
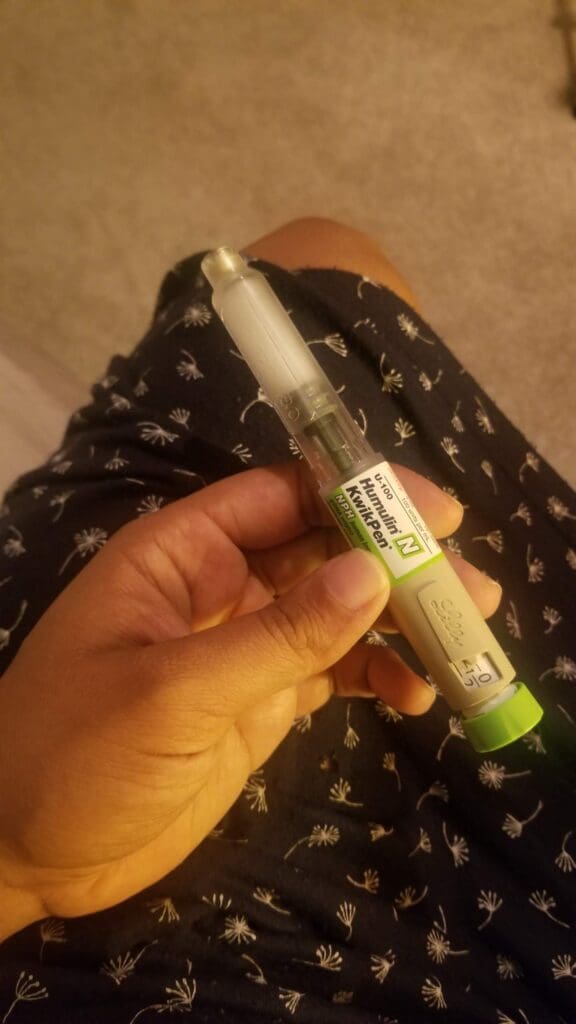
We met with doctors. We weighed options: oral medication (metformin) or injectable insulin. After research, I chose nightly insulin injections—I would inject myself in the stomach each night for the rest of the pregnancy. I hate needles, but of course I did whatever it took for a healthy pregnancy. I started at 8 units/night, and as the baby grew, that rose to 36 units/night. I have to say, injecting yourself in your growing belly is not something your body naturally wants you to do, it took several attempts each time.
Lifestyle Adjustments
Exercising and more specially adding a 10–15 minute walk after every single meal is really important, I would encourage that for everyone not just diabetics. I started maternity leave a few weeks early to reduce stress (because — yes — stress affects blood sugar). Timing of meals became rigid, and instead of just getting to eat things because “baby wants it or craves it” was no longer an excuse.
Diet Tips That Worked for Me
Here are some of the go-to meals and snacks that helped me:
Breakfast
Eggs + toast with butter or avocado. (No dairy or fruit in the morning → helped stabilize numbers.)
Snacks
- Cheese sticks (easy on the go)
- Fresh salsa (5 g carbs or less = “free food”) + tortilla chip dip
- Whole-wheat Melba toast or Triscuits + cottage cheese + sliced olives
- Almonds (in my purse at all times)
- Plain Greek yogurt with berries + nuts
Dinner
- Edamame pasta + mushrooms + minced meat + tomato sauce
- Cauliflower rice + chicken or minced meat stir-fry
- Fish tacos (corn tortilla within carb limits)
- Turkey chili (beans & corn in moderation)
- Protein-rich salads: Taco salad or Cobb salad (lots of protein, limited starchy veggies)
Bedtime snack
This was the toughest: they wanted ~14 g protein + ~15 g carb + ~5 g fat. I eventually settled on a protein shake (~30 g protein, 1 g sugar, 5 g carbs) plus a handful of almonds before bed as that was easiest. Because once the numbers dropped, the relief was significant.


Why This Matters
Gestational diabetes isn’t about being “lazy” or “eating too many sweets.” It’s a glucose‐intolerance condition that develops during pregnancy when your body can’t use insulin as efficiently. Extra sugar circulates, crosses the placenta, leads to elevated fetal blood glucose → triggers the baby’s pancreas to make extra insulin → extra energy gets stored as fat (which is not ideal).
And when you see your own numbers consistently high, it’s frustrating and emotional: disappointment, shock, the feeling that your body isn’t cooperating. You feel like you’re letting yourself and your baby down—even though you’re doing everything “right.”
After I delivered her, all my numbers went back to normal and I celebrated by eating a sandwich with white bread! I cried happy tears when I ate, checked my glucose monitor and all was normal again.
Final Thoughts
If you’re reading this and facing GD—whether diet‐controlled or insulin‐needed—you are not alone. You are not to blame. This is a condition of the body and hopefully temporary. With the right support, food planning, monitoring, movement and mindset, you’ll figure it out—just like I did.
Stay tuned for Part 2 (“Now”), where I’ll revisit this story from my perspective as a 40-year-old woman, now high‐risk pre‐diabetic, applying those lessons forward, bridging pregnancy past to present wellness.

Even though I didn’t always feel my best during that season — emotionally, physically, or mentally — I truly believe this chapter still deserves to be remembered. Pregnancy, even when it’s challenging is still a beautiful chapter of your story.
That’s why I always encourage mamas to document this chapter with a maternity session. Not because everything feels perfect — but because you are doing something extraordinary. You can see more details about the maternity experience I offer here → Maternity Photography
If this post resonated with you, I’d love to hear your story. Leave a comment below or reach out on Instagram at @reshmasondagar
Leave a Reply Cancel reply
Inquire here
I would love to answer any questions you may have and begin the planning process for your portrait session.
Let's capture this season of your life
© 2025 Reshma Sondagar
Navigate
Artist, Designer & Legacy Preserver serving Newport Beach, Laguna Beach and Orange County
Make your most loving
memories last
Follow along on Instagram